The Alliance for Health Policy and Systems Research works to improve the health of those in low- and middle-income countries (LMICs) by supporting the generation and use of evidence that strengthens health systems. As a partnership hosted by the World Health Organization, we work together with organizations around the world.
Message from the Board Chair
2024 was an important year for the Alliance, marking the beginning of a new strategic period focused on laying the foundations for impact, embedding research more deeply into country priorities, and forging innovative partnerships across the global health landscape.
At the Eighth Global Symposium on Health Systems Research in Nagasaki, Japan, I spoke about the urgent need to align health systems with the imperatives of planetary health. Climate change, political instability, and the lingering effects of the COVID-19 pandemic are challenging health system resilience worldwide. This moment calls for a paradigm shift towards systems that are informed by robust, context-specific research capable of advancing health and social justice.
This report showcases the Alliance’s unique value in generating and applying such research. Across the globe, the Alliance is supporting and advancing implementation research, strengthening capacities and creating conditions to improve policies and strengthen health systems. Whether it is studying health taxes, embedding research in country immunization strategies, or engaging policy-makers in research on climate and health, this report captures the projects taking shape and the effects they are already having as the Alliance begins implementing its 2024–2028 strategy, Aiming for impact.
This work is not done in isolation, but rather in partnership – with governments, research institutions and communities – ensuring that knowledge is not only generated but also used to transform policy and practice. At a time when the collapse of official development assistance for health threatens progress on health equity and health systems, this mission is more important than ever.
I thank the Alliance Board, its Scientific and Technical Advisory Committee, the Secretariat, funders, collaborators and the broader health policy and health systems research community for their contributions to the Alliance and for their dedication to strengthening health systems. The challenges ahead are immense, but so too is our collective capacity to meet them.
– Rt. Hon. Helen Clark
Chair of the Board, Alliance for Health Policy and Systems Research
Message from the Executive Director
In 2024, the Alliance moved to implement its new strategy – and the results are evident throughout this report. Across countries and topics, we have advanced work in each of our five focus areas, guided by our three strategic shifts – strengthening and scaling up impact, engaging more comprehensively with country priorities, and building new partnerships within the global health architecture.
We placed renewed emphasis on linking our work to tangible change. The structure of this report reflects that commitment. It is organized by our focus areas and spotlights how our projects have an impact by: shifting the frame, strengthening skills, changing practice, building connections, and informing policies and processes.
Aligned with our strategic shift to strengthen and scale up impact, the Alliance supported a growing portfolio of implementation-focused work designed to catalyse systems change. The MAINSTREAM initiative, for example, is working in six countries to embed learning into immunization programmes. In the area of noncommunicable diseases, implementation research in Ghana, Ethiopia, India and Nepal is improving chronic care delivery by supporting policy-makers to integrate research findings into service design. These efforts and more reflect our strategy’s emphasis on evidence-informed action.
To deepen relevance and responsiveness, the Alliance expanded support for research that is demand-driven, embedded in national processes, and tailored to specific country contexts. We supported eleven countries to understand the governance challenges of their national public health agencies and how they might be reformed, supporting research by the agencies themselves. We also initiated a multi-country effort to understand vaccine uptake, addressing both structural and behavioural drivers through context-specific strategies. These initiatives and others throughout the report illustrate how the Alliance is reorienting its support to be more locally led and attuned to country realities.
The Alliance also continued to broaden and diversify collaborations across institutions, sectors and regions. The Partnerships for stronger knowledge systems in Africa (KNOSA) initiative and the Policy-makers forum brought together diverse collaborators, fostering new relationships and shared agendas. Other projects facilitated peer learning, coordinated research efforts and enabled cross-country exchange.
Our work is made possible by the continued commitment of the governments of Norway, Sweden and the United Kingdom of Great Britain and Northern Ireland, as well as other significant partnerships, including with Gavi, the Vaccine Alliance, and the Gates Foundation among others, that have enabled us to launch critical new initiatives. From ministries of health to local institutions, colleagues at the World Health Organization and other partners and grantees – the progress captured in this report is the result of many contributions and I am deeply grateful to all who have played a role in advancing this crucial work.
– Kumanan Rasanathan
Executive Director, Alliance for Health Policy and Systems Research
A year in review
From research and reports to real-world use
Since its inception, the Alliance has helped generate understanding and evidence on strengthening health systems around the world. Through a growing body of peer-reviewed studies, teaching and training materials, and influential flagship reports, the Alliance has contributed frameworks, tools and insights that inform how health systems are studied and improved. These publications have played a pivotal role in building the field and integrating systems thinking into research and practice.
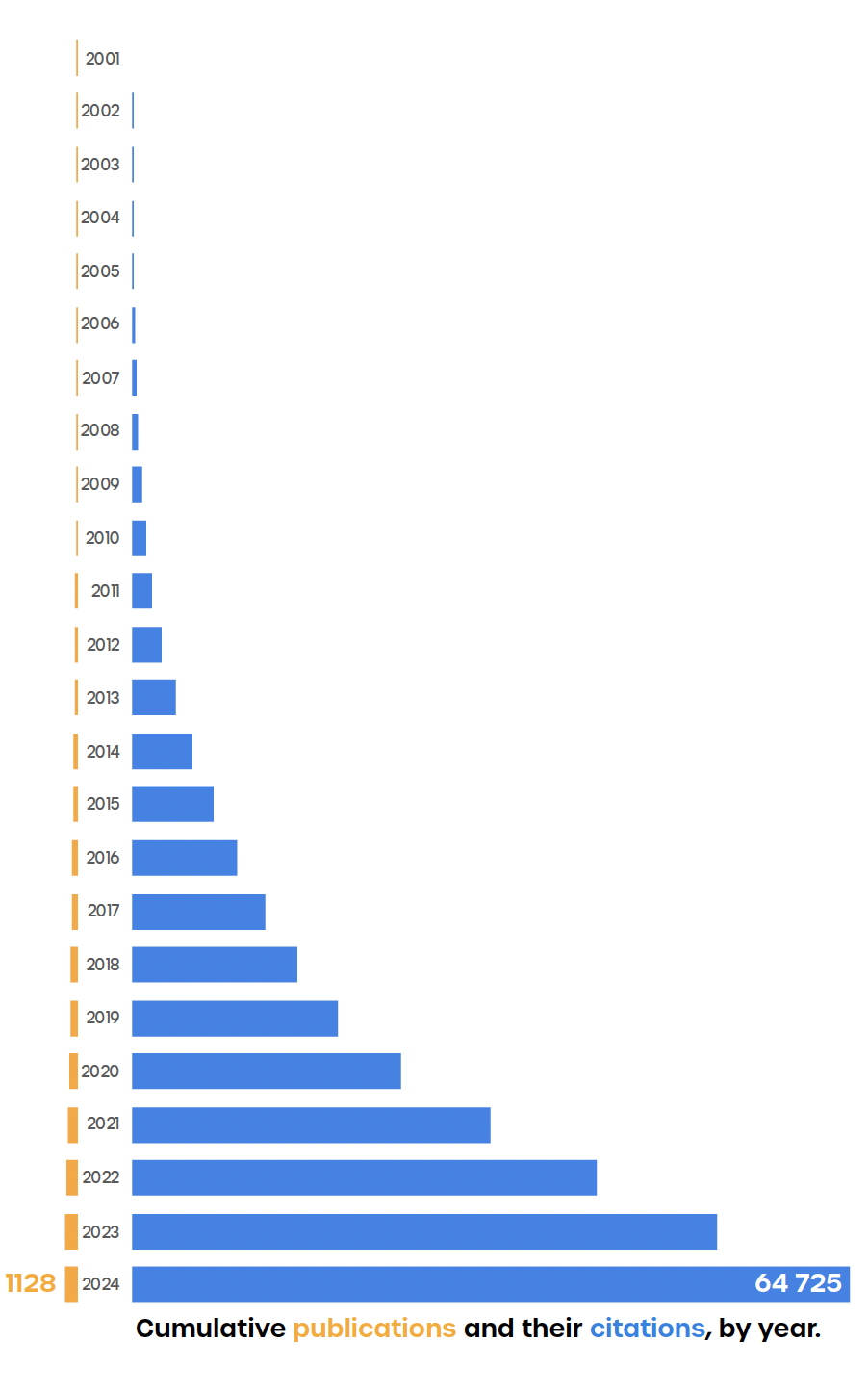
As of 2024, the Alliance has supported over 1100 publications, which have been cited around 65 000 times across academic and policy literature. In 2024 alone, Alliance-supported publications were cited nearly 12 000 times, underscoring the influential impact and significance of our work. The growing citation base is more than a measure of reach – it shows how ideas, approaches and studies championed by the Alliance have been used by the community.
A year in review
Select publications
The Alliance continued to produce and support high-quality, relevant publications that advance the field of health policy and systems research. These outputs reflect our commitment to co-producing knowledge with country partners, informing global health discourse, and contributing evidence that supports stronger, more equitable health systems
Health taxes: missed opportunities for health and financing healthcare by Helen Clark, Cathrine Lofthus, Robert Marten and Kumanan Rasanathan in The Lancet
Tying health taxes to health promotion is popular and effective in Thailand by Viroj Tangcharoensathien, Prakit Vathesatogkit and Supakorn Buasai in The BMJ
Political economy analysis of health taxes (tobacco, alcohol drink and sugar-sweetened beverage): qualitative study of three provinces in Indonesia by Abdillah Ahsan, Nadira Amalia, Krisna Puji Rahmayanti, Nadhila Adani, Nur Hadi Wiyono, Althof Endawansa, Maulida Gadis Utami, Adela Miranti Yuniar, Erika Valentina Anastasia and Yuyu Buono Ayuning Pertiwi in BMJ Open
Non-communicable diseases: can implementation research change the game for policy and practice? by Kumanan Rasanathan, Phyllis Dako-Gyeke, Wanrudee Isaranuwatchai, Yodi Mahendradhata, Morven Roberts, Giulia Loffreda, Sarah Rylance and Bente Mikkelsen in The Lancet
Prepared for the polycrisis? The need for complexity science and systems thinking to address global and national evidence gaps by Aku Kwamie, Sara Causevic, Goran Tomson, Ali Sie, Rainer Sauerborn, Kumanan Rasanathan and Ole Petter Ottersen in BMJ Global Health
Can current interlinked crises stimulate the structural and policy choices required for healthy societies? by Kumanan Rasanathan and Yogan Pillay in The BMJ
Comparing priority received by global health issues: a measurement framework applied to tuberculosis, malaria, diarrhoeal diseases and dengue fever by Rakesh Parashar, Sharmishtha Nanda, Stephanie L Smith, Zubin Shroff, Yusra R Shawar, Dereck L Hamunakwadi and Jeremy Shiffman in BMJ Global Health
Pathways to strengthen the climate resilience of health systems in the Peruvian Amazon by working with Indigenous leaders, communities and health officers by Claudia L Vidal-Cuellar, Victoria Chicmana-Zapata, Ingrid Arotoma-Rojas, Graciela Meza, James D Ford, Hugo Rodríguez Ferruchi, Elida De-La-Cruz, Guillermo Lancha-Rucoba, Diego B Borjas-Cavero, Sonia Loarte, Ofelia Alencastre Mamani, Victoria I Peña Palma, Maria G Coronel-Altamirano, Ivonne Benites, Giovanna Pinasco, Rosa Valera, Marco Maguiña Huaman, Adolfo Urteaga-Villanueva, César V Munayco and Carol Zavaleta-Cortijo in BMJ Global Health
Future proofing health in response to climate change and rapid urbanisation in Africa
by Monika Kamkuemah, Olalekan Ayo-Yusuf and Tolu Oni in The BMJ
Managing transitions from external assistance: cross-national learning about sustaining effective coverage by Zubin Cyrus Shroff, Susan P Sparkes, Ligia Paina, Maria Skarphedinsdottir, George Gotsadze, Henry Zakumumpa, Kun Tang, Prasadini N Perera, MyMai Yuan and Kara Hanson in Health Policy and Planning
Engaging non-state providers towards PHC in South Asia: considerations for policymakers by Zubin Cyrus Shroff, Anas Ismail, Kaosar Afsana, Manuj Weerasinghe and Krishna D. Rao in The Lancet Regional Health Southeast Asia
Understanding impact
Our current strategy, Aiming for impact, emphasizes laying the groundwork for and achieving impact as a guiding principle that shapes our work. While policy change is often seen as the primary measure of success, change can take many forms – all of which can contribute to stronger, more resilient health systems. In this report, we explore our strategic focus areas through five dimensions of change that reflect the range of ways that research can contribute to real-world improvements in health systems.
Shifting the frame
Changing how health systems issues are understood, discussed and solved
The research and dialogue that the Alliance supports can help shift how health systems issues are framed. Changing the way different stakeholders think and talk about a challenge can help elevate it on the political agenda or reveal new solutions.
Strengthening skills
Supporting institutions to generate, apply and implement health policy and systems research
The Alliance invests in national and local institutions, as well as broader knowledge ecosystems, to strengthen their ability to produce and use evidence in decision-making. Improved capacity enables research to be more relevant, timely and impactful.
Changing practice
Supporting practical changes in how services are delivered
Change does not happen through written policy or guidance alone. The way health practitioners and managers approach their work in their specific contexts has profound effects. Our focus on implementation research helps identify practical, context-specific solutions to improve health systems.
Building connections
Fostering peer learning and collaboration
The Alliance has a unique ability to convene stakeholders both within and across countries. We leverage this to foster peer-to-peer learning, experience exchange and new partnerships that help scale good practices and catalyse new ideas.
Informing policy and processes
Generating and applying evidence for better decision-making
We work with policy-makers and researchers to understand local challenges and support the production of politically feasible, evidence-informed solutions. This helps ensure that research leads to actionable recommendations and more responsive policies.
Transforming health systems
Strengthening health systems and services through a primary health care (PHC) approach remains central to the Alliance’s work to support countries in achieving universal health coverage (UHC). This includes generating evidence on how health systems can be better organized and financed – such as through the delivery of services for immunization and noncommunicable diseases (NCDs). Across multiple projects, we are co-creating learning agendas, embedding research into national systems, modelling the impact of different reforms and facilitating country-driven reforms grounded in local priorities.
Projects
India
Cameroon, Ghana, Madagascar, Malawi
Kenya, Nepal, Viet Nam, Sri Lanka
It is crucial to appreciate the constraints in which we work, and this is where modelling can help us optimize the performance of the health system in light of the constraints.
– Dr Kelechi Ohiri
Director-General of the
Nigeria National Health
Insurance Authority
Activities
Priority-setting workshops across all six MAINSTREAM countries, resulting in a synthesized list of priority implementation issues that are hindering local immunization programmes in reaching coverage and equity targets. These include identifying and reaching zero-dose children, addressing data quality and integration, alternative service delivery models and strategies for community engagement, which will be addressed via embedded implementation research projects.
Expert consultation on health policy and systems research for vaccine uptake held in April in Geneva (see meeting report), which informed the structure of a call for expressions of interest that was focused on reaching zero-dose children and addressing adolescent and adult vaccination across four health systems domains.
Expert consultation on modelling approaches and techniques to measure the impact of health systems strengthening interventions to provide essential health services, held in June in Geneva.
Published four country case stories from our implementation research studies on NCDs from Ethiopia, Ghana, India, and Nepal.
Impact
Alliance-supported research is already starting to shape ideas, relationships and decisions, even before final reports are published.
Shifting the frame
Through a series of co-creation processes – particularly on vaccine uptake and health systems modelling – stakeholders have redefined challenges through a systems lens. This shift in discourse is enabling more integrated, systems-oriented approaches.
Changing practice
In the MAINSTREAM initiative, six countries co-developed their research agendas through national workshops. Mentor institutes work alongside local teams, ensuring technical support and policy relevance. This model is helping institutionalize inclusive, collaborative research processes and building a network for sustainable demand and supply of implementation research that informs programmes and policies.
Building connections
New partnerships are a hallmark of this work. The Ethiopian Ministry of Health created a dedicated unit for evidence-informed policy-making – with support from the Alliance and the WHO Country Office for Ethiopia. National consortia for the modelling work are bringing together researchers, policy-makers and funders to co-design methods and set expectations from the start. Additionally, teams in each project are learning from each other’s setbacks and successes, accelerating innovation across countries.
Informing policies and processes
Karnataka state has shown interest in integrating PHC research insights into ongoing reforms. Ethiopia’s new policy unit is formalizing the use of evidence. In MAINSTREAM, WHO and Gavi, the Vaccine Alliance, are also engaged – applying learning and insights to their ongoing workstreams
Harnessing
digital health
Digital transformation holds the potential to improve health equity and strengthen primary health care. The Alliance is supporting research to understand how digital tools can enhance service delivery, empower users and support better decision-making. These studies are helping countries integrate digital health into national systems, informed by real-world evidence and close engagement with policy-makers.
Projects
Bhutan, Ethiopia, Georgia, Ghana, India, Indonesia, Pakistan, Zimbabwe
The problem is that we implement digital solutions on a project-by-project basis. We have too many verticalized thought processes – but health care is an interplay of many components.
– Professor Tungamirirai Simbini
University of Zimbabwe
Activities
Ten research teams completed their studies.
A synthesis workshop was held in June in Addis Ababa, Ethiopia, during which teams identified key evidence for advocacy and action at the national and subnational levels.
Impact
Alliance-supported research on digital transformation is contributing to policy shifts and system redesign. The work is helping countries understand how digital tools affect decision-making, service quality, and equity – and what’s needed for successful integration.
Informing policies and processes
A study on the Bhutan Vaccine System (BVS) – a nationwide digital intervention initially introduced to combat COVID-19 and since expanded to include human papillomavirus and influenza vaccinations – examined its role in vaccination delivery and citizen empowerment. Based on the study findings, the Ministry of Health updated the National eHealth Strategy and Costed Action Plan to address identified gaps – including digital infrastructure in remote areas, user training needs and interoperability. The research also influenced technical priorities within the Electronic Patient Information System (ePIS) and prompted calls for investment in solar-powered back-up systems for facilities with unstable electricity.
In Ghana, research focused on the District Health Information Management System (DHIMS) and Lightwave Health Information Management System (LHIMS), two overlapping digital health systems used for planning and reporting at the primary level. The study highlighted the operational burden caused by a lack of interoperability and digital literacy gaps among frontline users. In response, the Ministry of Health is considering establishing information and communication technology units in all facilities, hiring permanent information technology staff and accelerating the integration of the two systems – improving efficiency and strengthening digital governance at the national level.
Changing practice
One study evaluated the Georgian Birth Registry (GBR) and its role in improving continuity of care in antenatal and maternal services. The research led to practical improvements in how the registry is used – including updates to data fields, expanded training for data entry personnel and simplification of reporting forms. These adaptations have helped reduce administrative burdens and improve provider engagement with the system.
Preventing
noncommunicable diseases
The Alliance is supporting research and learning to prevent premature death and disability from noncommunicable diseases (NCDs), with a focus on primary prevention and the underlying social and commercial determinants of health. This includes generating policy-relevant evidence on the role of fiscal measures such as health taxes and setting new research agendas to advance health equity through multisectoral action.
Projects
Colombia, Egypt, India, Lebanon, Mongolia, Nigeria, Uganda, Zambia
Global
The Alliance focuses on multisectoral efforts and draws on strengths of health policy and systems research to address governance, policy development, and implementation to manage noncommunicable disease risks.
Activities
Worked with research teams in eight countries as they finalized their policy analyses on health taxes and prepared manuscripts for publication.
Supported grantees to conduct policy dialogues with health policy-makers in Lebanon, Mongolia and Zambia to explore opportunities for improving health taxes.
Convened a high-profile meeting in Geneva in October – with the Robert Wood Johnson Foundation, WHO and Boston University – bringing together over 40 global leaders to set an agenda for research and learning on social determinants of health equity.
Impact
Alliance-supported research on NCD prevention is influencing how fiscal policy and structural determinants are understood, debated and addressed – both at the country level, and within global policy circles.
Shifting the frame
The event held in Geneva is contributing to a shift in how research and learning on social determinants are conceived. Rather than focusing solely on identifying risks, participants called for approaches that challenge structural inequities and democratize knowledge production. Discussions highlighted the limitations of traditional research models – from overreliance on narrow methodologies to funding structures that exclude community-led work. The convening laid the groundwork for a new, action-oriented agenda – one that centres community participation, recognizes non-traditional knowledge systems and calls for applied, policy-relevant outputs.
Informing policies and processes
The Alliance’s BMJ Global Health supplement on framing health taxes continues to shape both national and international policy dialogue. Its analysis of political economy factors has been cited in key global policy platforms, including the 2024 task force report on health taxes supported by Bloomberg Philanthropies. By providing timely, evidence-informed framing, the research is helping position health taxes as a credible and actionable tool for reducing NCD risks.
Strengthening
climate
resilience
The Alliance is supporting research and learning that strengthens the resilience of health systems in the face of the climate crisis. This includes integrating health into climate mitigation and adaptation strategies, supporting countries to identify and prioritize actions, and advancing understanding of the health co-benefits of climate policies. Through cross-sector engagement and applied research, the Alliance is helping bridge the gap between health systems and climate action.
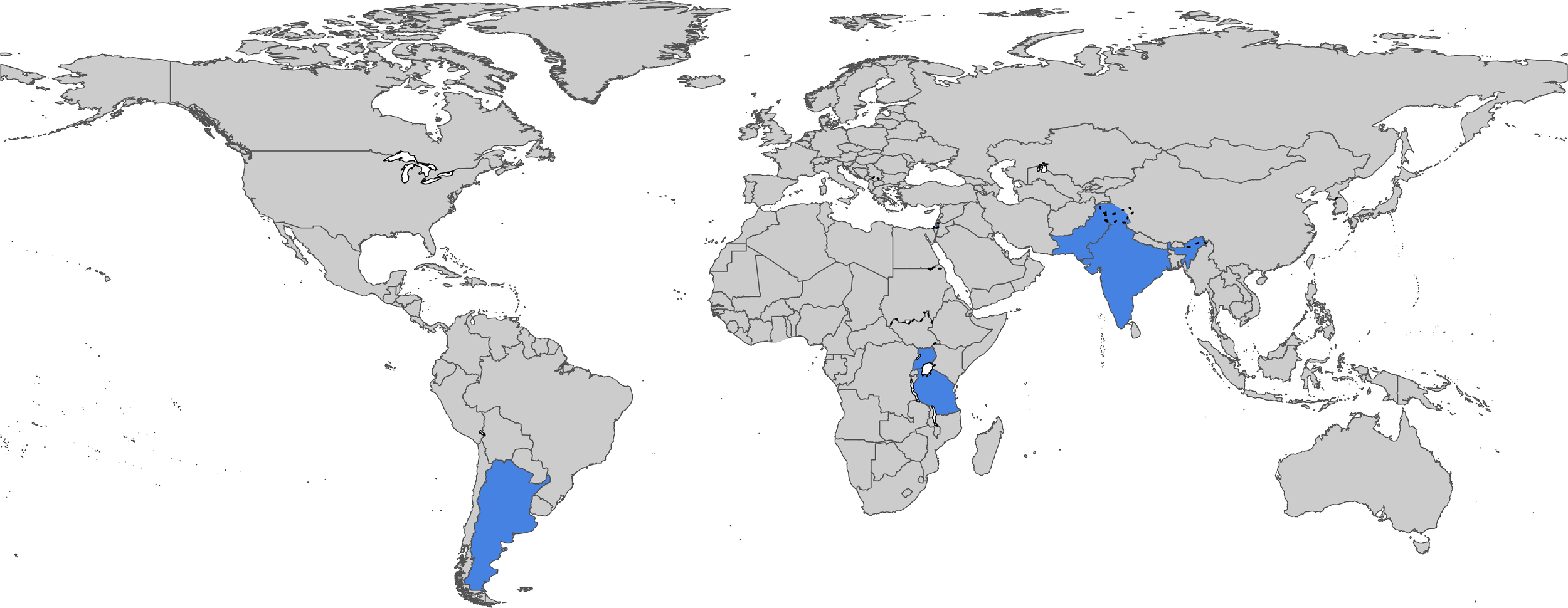
Projects
Argentina, India, Pakistan, occupied Palestinian territory including east Jerusalem, United Republic of Tanzania, Uganda
Global
Equity in climate change adaptation and resilience-building measures is essential to ensure that all communities, especially those with limited resources, have access to adequate health care and protection from climate-related health risks.
– Rt Hon. Helen Clark
Alliance Board Chair at HSR2024 in Nagasaki, Japan
Activities
Conducted collaborative workshops in Kuala Lumpur, Malaysia, and in Montreux, Switzerland, bringing together global experts to explore actionable pathways for realizing health co-benefits from climate adaptation and mitigation strategies, in collaboration with WHO and the United Nations University International Institute for Global Health.
Supported research teams in six countries as they finalized their studies on climate-resilient health systems, contributing to national policy processes such as Health National Adaptation Plans (H-NAPs).
Impact
Alliance-supported research on NCD prevention is influencing how fiscal policy and structural determinants are understood, debated and addressed – both at the country level, and within global policy circles.
Alliance-supported research is helping position health systems not only as responders to the climate crisis but also as contributors to mitigation and broader sustainable development goals. The work is informing national planning processes, strengthening cross-sector dialogue, and advancing a new research agenda at the intersection of climate and health.
Shifting the frame
The Alliance is helping reframe climate policy as an opportunity to improve, not just protect, health. Through its work on health co-benefits, the idea that mitigation and adaptation strategies – in sectors like food, energy and transport – can actively advance health outcomes is gaining traction. A global workshop in Montreux helped identify policy openings in countries such as Argentina and Mozambique, where health can be embedded more prominently in national climate strategies, marking a shift toward more integrated, multisectoral action.
Informing policies and processes
In India, Uganda and the United Republic of Tanzania, research teams contributed to the development of H-NAPs. These contributions are helping shape national responses to climate-related health threats and demonstrate the value of health policy and systems research in identifying context-specific priorities and feasible adaptation strategies.
Preparing for and responding to emergencies
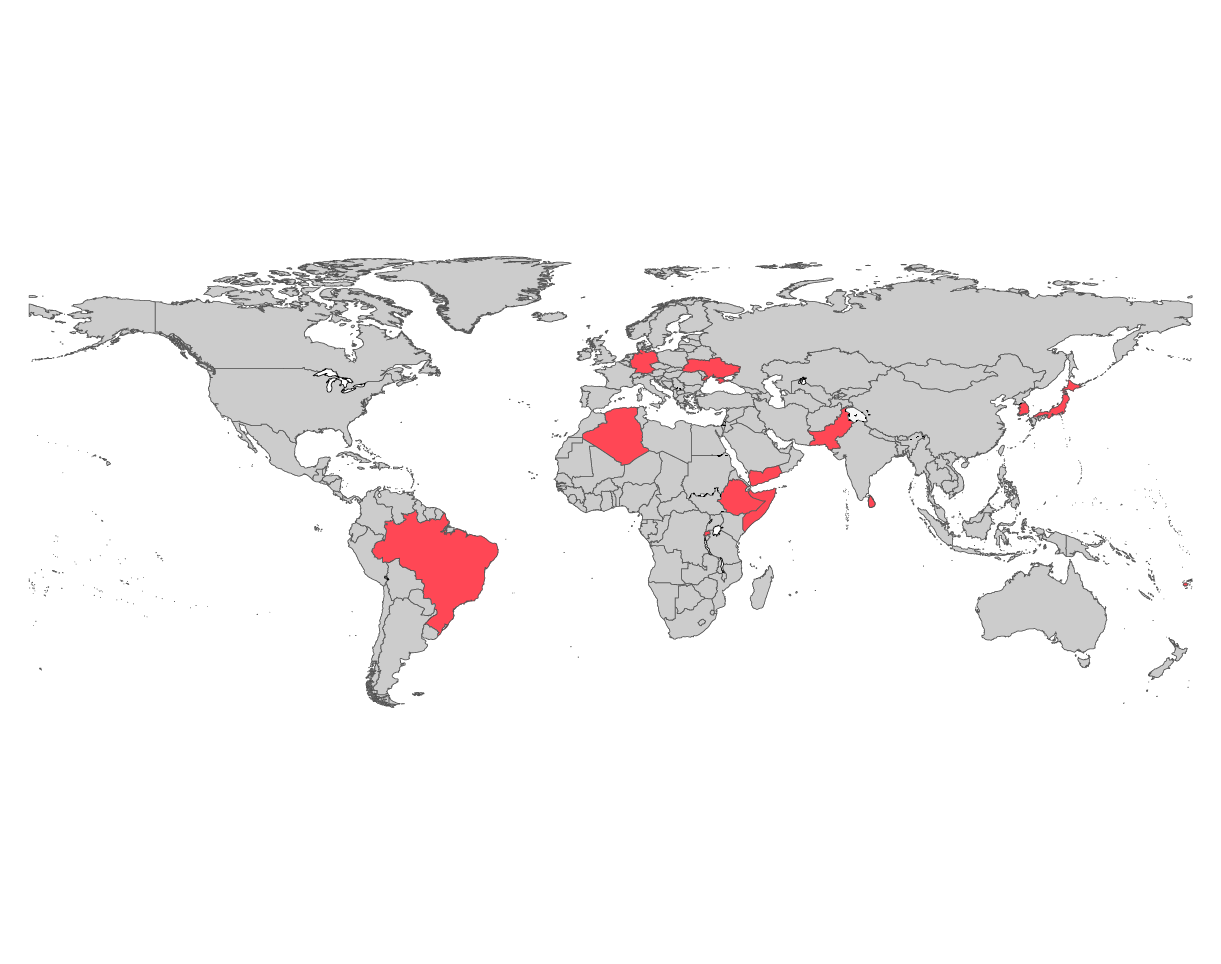
The Alliance is supporting learning for emergency preparedness and response with research in two areas: effective governance and coordination of national public health agencies (NPHAs) and the delivery of health services in conflict-affected settings. Through these efforts, the Alliance is helping countries build more resilient health systems that are better equipped to prevent, prepare for and respond to public health emergencies, including in fragile and protracted crisis environments.
Projects
Somalia, Ukraine, Yemen
Algeria, Brazil, Ethiopia, Fiji, Germany, Japan, Pakistan, the Republic of Korea, Rwanda, Singapore, Sri Lanka
According to WHO, nearly a quarter of the global population currently lives in settings affected by conflict, displacement and natural disasters. Improving governance and performance of national public health agencies in these settings is essential to build more resilient health systems.
Activities
Convened a consultation in May with participation from the WHO Emergencies Programme, policy-makers and global experts to discuss governance models for national public health agencies during health emergencies, co-hosted with Singapore’s Interim Communicable Diseases Agency.
Conducted a scoping review on the enablers and barriers to policy-maker engagement in health emergency research, informing the research themes for the NPHA Governance Learning Network.
Received expressions of interest from NPHA representatives from 11 countries in the research and learning programme, submitting proposals on themes like partnerships, legal mandates, NPHA-Ministry of Health relationships, and using research to enhance NPHAs’ emergency response.
Supported the selection and onboarding of research teams in Somalia and Yemen to begin studies on health service delivery in conflict zones.
Impact
For this new area of work, the emphasis has been on building networks, co-developing research agendas, and creating spaces for peer exchange – laying the foundation for stronger systems and more connected responses to future health emergencies.
Building connections
The Alliance helped establish a new National Public Health Agencies Governance Learning Network, bringing together 11 agencies, academic institutions and global experts to co-create evidence and share strategies for emergency preparedness and response. Sparked by a consultation in Singapore and a scoping review on research–policy engagement, the network is creating a space for peer exchange, mutual support and collective reflection on governance challenges – from institutional mandates to inter-agency coordination. This learning and knowledge-sharing platform is helping define how national leaders, international organizations, and funders can support more effective governance – and how recent reform experiences can be translated into actionable strategies across contexts.
Aligning
knowledge
ecosystems
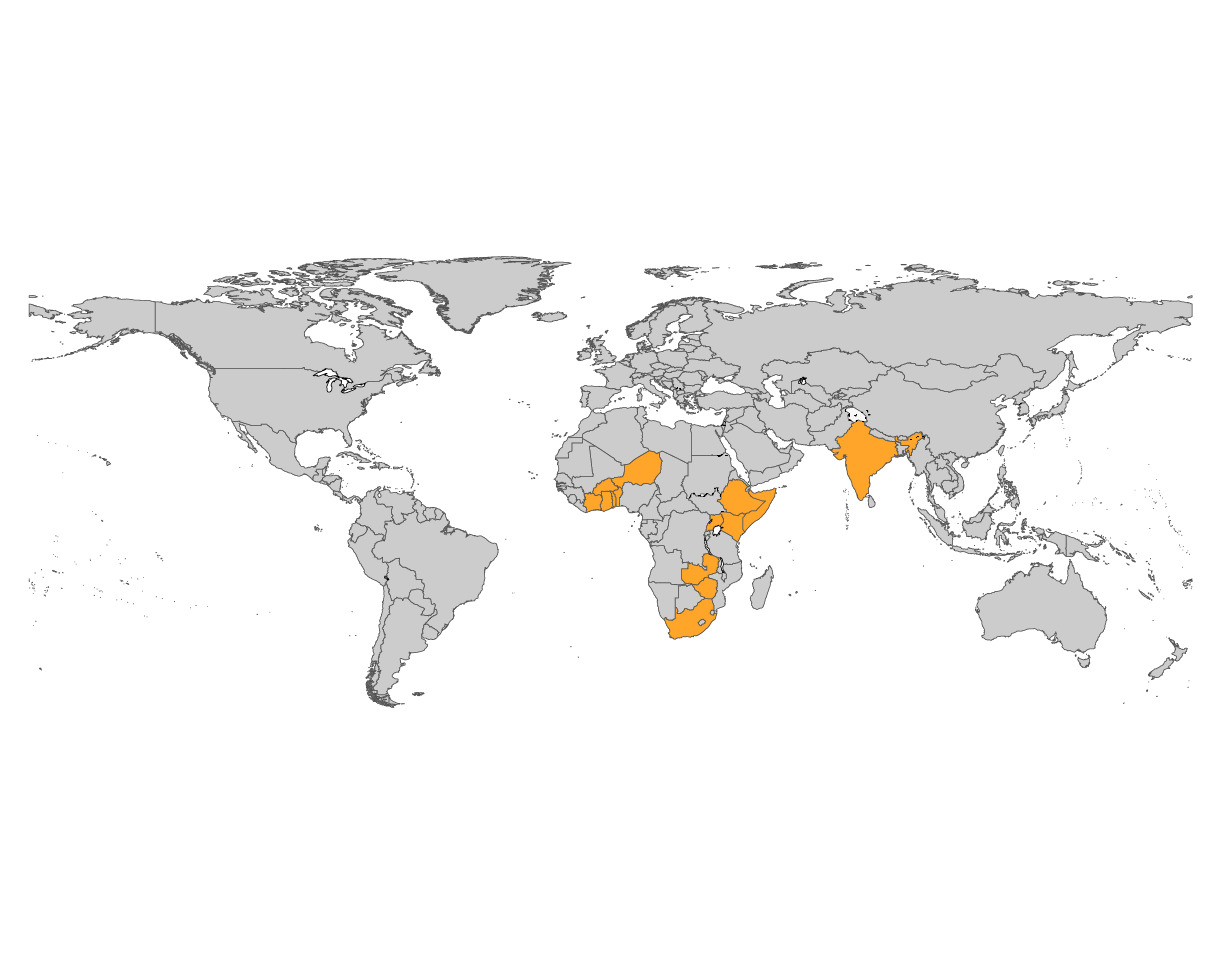
The Alliance has sharpened its approach to capacity strengthening by shifting from a focus on individual training to a broader emphasis on institutional engagement, systems change and policy-maker involvement. Through new and continuing initiatives, the Alliance is helping build research ecosystems that connect evidence generation to policy and practice – particularly in under-represented contexts such as francophone Africa and fragile settings. By fostering peer networks and documenting real-world learning, these efforts aim to ensure sustainable research leadership, policy engagement and long-term impact.
Projects
Benin, Burkina Faso, Côte d’Ivoire, Niger, Togo
Ethiopia, Kenya, Somalia, Uganda
South Africa
Burkina Faso, Ghana, India, Kenya, Uganda, Zambia, Zimbabwe
This mentorship programme enables my country to have a qualified expert in the field of research on health policies and systems, producing high-quality data that can be utilized [for policy]. At the end of this programme, we aim to integrate this training into the master’s programme at the Nazi Boni University in Bobo Dioulasso.
– B. Leticia Delphine Sakana
CRESPA fellow from Burkina Faso
Activities
Organized an in-person training workshop in Ouagadougou, Burkina Faso, for six CRESPA fellows, supported by quarterly webinars for project updates and cross-disciplinary discussions.
Supported a sense-making workshop in the Western Cape about its use of the systems for health approach, gathering district health managers from six provinces to review lessons learned from South Africa’s health system strengthening efforts.
Held the KNOSA inception co-creation workshop in Addis Ababa, Ethiopia, bringing together policy-makers, researchers and global experts to discuss knowledge systems strengthening and support the refinement of their proposals.
Completed a reflective session at the Eighth Global Symposium on Health Systems Research on the two rounds of the HPA Fellowship, leading to the publication of key articles and a scoping review on the evolution of health policy analysis literature.
Impact
The Alliance’s focus on institutional and systems-level capacity strengthening is yielding results – from embedding HPSR training into university curricula to establishing platforms for cross-country learning and collaboration. Rather than short-term skill-building, these programmes are fostering the networks, relationships and systems needed to sustain research and policy engagement over time.
Strengthening skills
Through programmes like CRESPA, the Alliance supported institutions to develop and deliver new HPSR training, generate original research, and advocate for greater incorporation of HPSR in academic programmes. In francophone Africa, six CRESPA fellows trained 149 graduate students in five countries, while also engaging institutional leadership to embed HPSR into academic offerings. These efforts represent a shift from one-off training to deeper, more sustainable institutional capacity strengthening – helping to ensure local ownership, continuity, and long-term impact in health systems research and policy.
Building connections
Programmes like KNOSA and MAST are strengthening the bonds between researchers, institutions and policy-makers. In East Africa, KNOSA teams are already supporting the enhancement of national knowledge systems. The inception workshop in Addis Ababa also supported collaboration and knowledge sharing across borders. In South Africa, long-standing relationships between health departments and researchers are informing peer learning across provinces.
Engaging strategically
Effective engagement is a core part of transforming evidence into impact. It’s not just about sharing research – it’s about creating dialogue, building trust, and making knowledge accessible and actionable for those shaping health systems. Through communications and strategic engagement initiatives, the Alliance amplified research and fostered collaboration across policy, practice and research communities. By participating in and convening major global health events, and launching a new alumni platform, and convening global policy-makers, we helped strengthen connections and highlight the role of health policy and systems research on the global stage.
Projects
What made the Alliance Policy-makers Forum truly special was the sense of openness and trust we cultivated together, allowing us to bring our diverse experiences to the table. We were able to move from a space of understanding shared challenges to co-creating a network to help each other think through them.
– Dr Keith Cloete
Head of the Western Cape Department of Health and Wellness in South Africa, Forum Facilitator
Activities
Launched a supplement on rethinking external assistance for health at the Prince Mahidol Award Conference in Bangkok, Thailand.
The inaugural Alliance Policy-makers Forum was convened in October in Geneva, Switzerland, with participation from policy-makers from eight countries.
Introduced a new Thinker in residence programme, with Dr Seye Abimbola the first appointee, to foster innovative approaches and fresh ideas.
Convened a side event during the 77th World Health Assembly in Geneva, Switzerland, on the role of research and evidence in achieving the SDGs. Discussions highlighted the need to invest in national research capacity and communicate the value of research as critical paths to achieving the Sustainable Development Goals.
At the World Health Summit in Berlin, Germany, the Alliance joined the celebrations for Professor Lucy Gilson, who received the 2024 Virchow Prize for her work towards more sustainable and people-centred health systems. Additionally, the Rt Hon. Helen Clark contributed an article for the edited collection, Health: a political choice, emphasizing knowledge generation as a way to engage with the inherently political nature of health policy.
Co-sponsored the Eighth Global Symposium on Health Systems Research in Nagasaki, Japan, where we organized five satellite sessions, two capacity-strengthening sessions, and three organized panel discussions. The Rt Hon. Helen Clark delivered a plenary address, and the Alliance co-hosted a reception marking the 20th anniversary of the Mexico Ministerial Summit on Health Research.
Formally launched the Alliance Alumni Network to support ongoing engagement and collaboration.
Impact
By shaping conversations at major global health events, celebrating leaders in the field, and deepening community connections, we contributed to shifts in thinking and practice. Our efforts reinforced the importance of health policy and systems research in driving change and demonstrated how sustained engagement can influence both discourse and collaboration.
Shifting the frame
Through high-level engagements, the Alliance helped position health policy and systems research as integral to global debates on sustainable development, planetary health and the future of development assistance. More than an individual honour, having the 2024 Virchow Prize go to a champion for the field of health policy and systems research highlights its growth and evolution over the past 25 years.
Building connections
The Alliance Alumni Network laid the groundwork for a more connected HPSR community, strengthening ties between researchers, policy-makers, and practitioners worldwide. The Policy-makers Forum is creating new space for national leaders to engage. By convening shared spaces at key events and celebrating longstanding partnerships, the Alliance reinforced its role as a bridge-builder in the field. .
2024 donors
The Alliance gratefully acknowledges core financial support in 2024 from the Norwegian Agency for Development Cooperation (Norad) and the Swedish International Development Cooperation Agency (Sida).
The Alliance also acknowledges significant ongoing programme support from the Gates Foundation; the Department of Health and Social Care, United Kingdom of Great Britain and Northern Ireland; and Gavi, the Vaccine Alliance.
We also received specified funding from the Federal Republic of Germany, the Medical Research Council and the Robert Wood Johnson Foundation.
Governing bodies
Alliance Board
CHAIR, Helen Clark, Former Prime Minister,
New Zealand
VICE CHAIR, Jeanette Vega, Former Minister of Social Development and Family, Chile
Jeremy Farrar, Chief Scientist, World Health Organization, Switzerland
Rubayat Khan, Director, Health Programs, Endless Network
Gabriel Leung, Executive Director (Charities and Community), Hong Kong Jockey Club
Anders Nordström, Ambassador for Global Health, Ministry of Foreign Affairs, Sweden
Ingvar Theo Olsen, Policy Director, Department for Global Health, Education and Research, Norwegian Agency for Development, Norway
Teresa Soop, Senior Research Advisor, Swedish International Development Cooperation Agency, Sweden
Eren Zink, Senior Research Advisor, Swedish International Development Cooperation Agency, Sweden
Scientific and Technical Advisory Committees
CHAIR, Helen Schneider, Professor, School of Public Health, University of the Western Cape, South Africa
Octavio Gómez Dantés, Senior Researcher, Center for Health Systems Research, National Institute of Public Health of Mexico
Karen Grépin, Associate Professor, School of Public Health, University of Hong Kong, China, Hong Kong SAR
J. Jaime Miranda, Professor and Head of Sydney School of Public Health, University of Sydney, Australia and Research Associate, CRONICAS Center of Excellence in Chronic Diseases, Universidad Peruana Cayetano Heredia, Peru
Sudha Ramani, Independent Consultant, Health Policy and Systems Research, Mumbai, India
Emma Sacks, Associate Faculty, Department of International Health, Johns Hopkins Bloomberg School of Public Health, United States of America
Amirhossein Takian, Vice Dean, School of Public Health, Tehran University of Medical Sciences (TUMS), Islamic Republic of Iran
Benjamin Tsofa, Senior Principal Research Scientist - Health Policy and System Research, KEMRI-Wellcome Trust Research Programme / KEMRI Centre for Geographic Medicine Research, Kenya
Alliance Secretariat
Kumanan Rasanathan, Executive Director
Luzviminda Diaz Caguioa, Team Assistant
Livia Dal Zennaro, Technical Officer
Ana Lorena Guerrero Torres, Technical Officer
Anas Ismail, Young Professional (Health Systems Research)
Amanda Karapici, Young Professional (Health Systems Research)
Jeffrey Knezovich, Technical Officer
Aku Kwamie, Technical Officer
Kaung Suu Lwin, Young Professional (Health
Systems Research)
Robert Marten, Strategy and Partnership Officer
Karin Miyamoto, Junior Professional Officer
Daniela Rodriguez, Scientist (Implementation Research)
Idil Shekh Mohamed, Junior Professional Officer
Meike Schleiff, Scientist
Zubin Shroff, Technical Officer
Kanika Sokchea, Administrative Officer
John Warriner, Technical Officer
Yasmine Yahoum, Team Assistant
Note: People listed in this section served on the Board or STAC or were staff members employed by the Secretariat at some point during 2024. They do not necessarily reflect the current composition of these bodies.