The Alliance for Health Policy and Systems Research works to improve the health of those in low- and middle-income countries (LMICs) by supporting the generation and use of evidence that strengthens health systems.
As an international partnership hosted by the World Health Organization, we work together with organizations around the world.

* Most figures based on those grantees that responded to the annual survey
Message from the Board Chair
As health policy and systems research (HPSR) becomes increasingly important for improving health around the world, I am proud of the Alliance’s ongoing support of this quickly evolving field. This report highlights the ways in which the Alliance championed HPSR in 2018 – from investing in future HPSR leaders to building relationships and pushing the boundaries of the field. But we also need to keep one eye to the future to ensure we are best positioned to meet the challenges and opportunities ahead.
2018 was the 40th anniversary of the Alma-Ata Declaration, and with its enduring commitment to Health for All, we see that the goals that underpin the development of health systems have endured. However, contexts and priorities have changed, research methods have progressed, and health organizations have continued to learn and to adapt.
As we look at the big challenges for global health, climate change looms large, with environmental degradation leading to ill health in multiple ways; on one hand, air pollution is having an impact on human health, on the other shifting weather patterns are contributing to food insecurity. Migration and refugee crises are changing the way we think about how health systems are organized. We also see emerging and re-emerging diseases and a growing threat of antimicrobial resistance. Each of these trends reinforce each other and concentrate their harms on the most vulnerable populations.
These challenges are not limited to any specific field, even one as broad as HPSR. The Sustainable Development Goals (SDGs) recognize this and prioritize working across sectors to face these challenges. This is an opportunity for the HPSR community to lead, given its pioneering work on systems thinking, its focus on health equity and the strength of its multi-disciplinary approaches.
As an early and committed champion of HPSR, the Alliance remains in a strong position to help the wider HPSR community to face these challenges. The Alliance Board, those on the Scientific and Technical Advisory Committee (STAC), the Alliance Secretariat, and the Executive Director, Abdul Ghaffar, have all helped to assure that.
As the World Health Organization begins its transformation process, this is also an opportunity for me to thank Assistant Director General Dr Naoko Yamamoto for the dedication to and oversight of the Alliance that she has provided in 2018. In the future, the Alliance will form part of the Science Division under the stewardship of the new Chief Scientist, Dr Soumya Swaminathan, which will further bolster the Alliance’s
research activities.
– DAVID PETERS
Message from the Executive Director
As I look back on 2018, I am struck by all the hard work emerging from the Alliance Secretariat and its grantees – work that has continued to advance the field of health policy and systems research in various ways. One of our focus areas has been working to stimulate policymaker demand and use of relevant evidence, and working with researchers to respond appropriately to that demand. Our main approach to this has been embedding research into decision-making processes – whether it is through implementer-led projects or by developing platforms in ministries of health to support rapid evidence synthesis.
In line with the World Health Organization’s new General Programme of Work, we have been working closely with countries to ensure our approaches are driven by local demand. As part of an initiative spearheaded by the WHO Chief Scientist, we have worked directly with the governments of Nepal, India and Ethiopia to shape the research that underpins their universal health coverage (UHC) initiatives as they work toward SDG 3.
Equity has also been a major pillar of our work. Following a stakeholders meeting in Dubai at the beginning of 2018, we have launched a capacity building initiative on gender and intersectionality. Our commitment to promoting women leaders in HPSR is demonstrated in all our projects – which require at least 50% of team members are women – and through specific initiatives, such as publication mentorship. I’m pleased that this year we are also able to start reporting on the gender breakdown of a few key statistics, like lead authorship of peer reviewed publications (see 2018 by the numbers). We are committed to collecting, and reporting, on further data that takes into account gender and other forms of historic advantage and disadvantage.
Working with partners, we made significant contributions to new knowledge in 2018 by publishing valuable articles, guides, readers and other resources. This includes a reader designed to encourage and deepen health policy analysis work in low- and middle-income countries (LMICs), a methods guide on evidence synthesis, and a journal special issue on understanding the role of non-state providers in achieving UHC.
Finally, I would be remiss not to note the Fifth Global Symposium on Health Systems Research, of which the Alliance is a co-sponsor, as a highlight of the year. It was a highlight not just for the Alliance, which had a strong presence there in Liverpool (see page 6), but for the wider HPSR community and for the organizers at Health Systems Global. Ensuring there are opportunities for HPSR practitioners – from researchers to policymakers to practitioners and knowledge brokers – to foster connections remains a priority in our field.
– ABDUL GHAFFAR
We bring
people together.
Cultivating the health policy and systems research (HPSR) community is as important as developing the HPSR field. That is one reason why the Alliance fosters networks, establishes platforms and convenes different groups.
Some of these networks, like the LEAP Forum, seek to steer the field, while others bring together groups that might not otherwise interact to help expand their connections. Providing opportunities for shared learning and discussion is also critical – this can reinforce our work building the capacity of health systems leaders.

Bringing people together
In 2018, the Alliance:
GLOBAL EVIDENCE SYNTHESIS INITIATIVE (GESI)
“It takes a system to save a life – not any system but one that relies on solid evidence.”
— DR SHAWKY AMINE EDDINE
— DR SHAWKY AMINE EDDINE
The Alliance played a key role in founding the Global Evidence Synthesis Initiative (GESI), which helps LMICs countries to build the capacity to generate and use research synthesis to enhance public policy and service delivery.
One of the hallmarks approaches being developed through this consortium is the early and active engagement of policymakers in identifying priorities for syntheses to ensure they respond to current needs. The GESI Network currently consists of 46 centres from 24 LMICs from across the globe. In 2018, GESI organized sessions at global conferences and hosted a series of webinars on evidence synthesis and the use of review findings to support policy and practice.
LEARNING ENGAGING AND ADVOCATING FOR POLICY AND SYSTEMS RESEARCH (LEAP) FORUM
Connecting the health systems research, policy and implementation communities for better coordination of efforts.
For the last two years, the Alliance has coordinated a network of networks that work on HPSR: the Learning Engaging and Advocating for Policy and Systems Research (LEAP) Forum. LEAP is a platform for collaborative problem-solving and discussing ways of generating and using policy-relevant knowledge.
LEAP builds on gains the Alliance has already made in working with policy- and decision- makers and other partners in different regions to identify barriers and incentives to using evidence. The LEAP Forum met at the Symposium in Liverpool and agreed that a full meeting would take place in 2019.
PRIMARY HEALTH CARE MEASUREMENT AND IMPLEMENTATION RESARCH CONSORTIUM
Together we can and will achieve health and well-being for all, leaving no one behind.
The Alliance has partnered with Ariadne Labs and Harvard T. Chan School of Public Health to develop a Primary Health Care Measurement and Implementation Research Consortium. Launched in Liverpool, the consortium convenes researchers and policymakers from multiple disciplines and representing academic institutions, government agencies, international organizations and non-governmental organizations to accelerate progress in primary health care (PHC) research in LMICs.
The goal is to develop a robust PHC global research network structure and to secure the resources needed to carry out prioritized and policy-relevant PHC research. The ultimate intent is to support better measurement, implementation and improvement efforts in priority areas for PHC in LMICs. Funded by the Gates Foundation, initial PHC studies are being undertaken by George Washington University, American University of Beirut, Stellenbosch University, The George Institute for Global Health and the World Organization of Family Doctors.
We empower leaders.
Health policy and systems research is an emerging and evolving field that needs more champions around the world.
The Alliance works with researchers and policymakers to enhance their HPSR skills – especially around generating useful evidence and employing that evidence in decision-making processes. We work at both the individual and institutional levels to strengthen the HPSR environment in many countries.

Empowering leaders
In 2018, the Alliance:
Embedding RApid Reviews in Health Systems Decision-Making (ERA) initiative
Rapid reviews of health policy and systems evidence can provide relevant and actionable evidence at every step of the decision-making process.
The Embedding RApid Reviews in Health Systems Decision-Making (ERA) initiative embeds rapid review production directly within health decision-making institutions in LMICs. Four ERA platforms have been established in Georgia (Parliament of Georgia, Healthcare and Social Issues Committee), India (National Health Systems Resource Centre, Ministry of Health and Family Welfare), Malaysia (Ministry of Health, National Institutes of Health, Institute for Health Systems Research) and Zimbabwe (Ministry of Health and Child Care). All countries selected committed to co-funding the ERA activities through in-kind and/or financial support.
The ERA platforms benefit from scientific support provided by a technical assistance centre – a consortium between Makarere University (Uganda) and the University of Toronto (Canada) – with the Alliance. The Alliance convened a workshop in July 2018 in Kuala Lumpur, Malaysia, with decision-makers and researchers to devise a strategy to establish the ERA platforms and stimulate demand and uptake of rapid syntheses of health policy and systems evidence in LMICs.
Health Policy Analysis (HPA) Mentorship Programme
The Alliance has invested in a group of Health Policy Analysis (HPA) Fellows, who are LMIC-based PhD students working with world leaders to develop their skills. Nine Fellows were selected for this programme, the majority of whom are women. After an initial protocol development workshop in December 2017, they have been working on their research studies, incorporating an HPA lens into their doctoral theses.
The HPA Fellows had a strong presence in Liverpool, where some of the fellows presented their findings and analyses during two organized sessions. An additional workshop brought together these fellows in Cape Town, South Africa, at the end of 2018 to reflect on progress of their work. The research resulting from this programme will culminate in a series of articles planned for 2019.
Mentorship scheme for early-career women to improve publication skills
"This programme provides female researchers from LMICs an opportunity to be heard and acknowledged for their work."
— MEHR MANSOOR, MENTEE
— MEHR MANSOOR, MENTEE
Peer-reviewed publications are important for communicating scientific work, gaining recognition within the research community and career progression. However, women in academia often lag behind their male colleagues in publications. There are many potential reasons for this, and women often face unique challenges, including competing professional and personal roles, and difficulties navigating male-dominated work environments. This programme hopes to address these challenges through targeted support from experienced mentors.
In 2018, we selected 10 mentees who are working with nine mentors from around the world to develop their research into peer-reviewed journal articles. They have benefited from a joint webinar and as well as personal guidance on their articles from their mentors.
We advance knowledge.
The Alliance supports a number of ongoing research projects around the globe. These research portfolios help us to generate knowledge and to advance understanding in two critical realms: specific health systems topics, and the field of health policy and systems research.
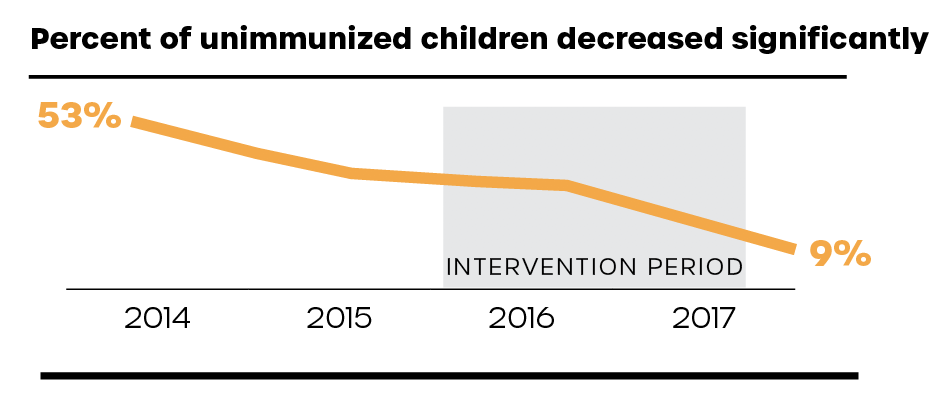
For example, one group of embedded implementation research projects supported by UNICEF and Gavi, the Vaccine Alliance focuses on improving immunization rates. Research findings from these projects provide information relevant to the field of immunization but also broaden the understanding of health systems structures and barriers to access.

Advancing knowledge
Evidence synthesis for health policy and systems: a methods guide
"[This guide] will prove useful to researchers and decision-makers everywhere as they seek to play their part in promoting health, keeping the world safe and serving the vulnerable."
— DR TEDROS GHEBREYESUS, DIRECTOR GENERAL, WORLD HEALTH ORGANIZATION
— DR TEDROS GHEBREYESUS, DIRECTOR GENERAL, WORLD HEALTH ORGANIZATION
Evidence Synthesis for Health Policy and Systems: A Methods Guide provides a rationale for synthesizing evidence from HPSR to support health policy-making and health systems strengthening. It introduces key challenges in synthesizing HPSR evidence and provides guidance on addressing these issues.
This guide examines various synthesis methods – quantitative, qualitative and mixed methods – and provides practical guidance to engage decision-makers in evidence synthesis, enhance the policy relevance of syntheses, and foster the uptake of review findings in policy and practice. The guide was introduced at the Fifth Global Symposium on Health Systems Research in 2018 to a standing-room-only crowd. All hard copies available were distributed there, and the guide was downloaded over 250 times from the Alliance website in the month of October alone.
A health policy analysis reader: The politics of policy change in low- and middle-income countries
"[It] gives insights about the challenges of changing policy and ideas about how to support policy change."
— DR LUCY GILSON, UNIVERSITY OF CAPE TOWN
— DR LUCY GILSON, UNIVERSITY OF CAPE TOWN
A Health Policy Analysis Reader: The Politics of Policy Change in Low- and Middle-income Countries aims to encourage and deepen health policy analysis work in LMICs. It illuminates the range of health policy analysis studies that have been conducted in LMICs, highlights relevant theories and points to new directions for such work.
The reader includes methodological and analytical pointers and includes considerations about how to use health policy analysis prospectively to support health policy change. It was launched during the Symposium in Liverpool, and despite its heft, all available hard copies and soft copies were distributed.
Special issue of the International Journal of Equity in Health
Moving towards universal health care: engaging non-state providers
One of the article collections supported by the Alliance this year was a special issue of the International Journal of Equity in Health. It focuses on the role of non-state providers of health (NSPs) in achieving UHC.
This publication pulls together seven country case studies and a cross-country study that examines what lessons can be drawn for effective contracting of NSPs in LMICs by governments keen to explore ways to move more efficiently and effectively towards UHC.
We inform policy.
The Alliance prides itself on developing projects that link research, policy and practice. One project design that has proved very successful in this respect is embedded implementation research. In these projects, policymakers work directly with researchers on a health systems challenge that they are trying to resolve. In some cases, the policymakers may even be the research lead. This partnership enables effective policy implementation at the local level.
But it isn’t just at the local level where the Alliance has informed policy. Research from the Alliance and our grantees has fed into global guidelines and discourse as well as national policy processes.

Informing policy around the world
GEORGIA
The Alliance supported the establishment of an embedded rapid review platform within the Parliament of Georgia’s Healthcare and Social Issues Committee, which is stimulating demand for evidence for Regulatory Impact Assessments (RIAs) and health policy-making.
ETHIOPIA
The Alliance review centre based at Jimma University supported the Ethiopian Ministry of Health in establishing a Policy Analysis Case Team (PACT), which is now commissioning policy briefs, rapid reviews and primary research. Policymakers reported an “interest to embed the rapid review methods in policy planning among high level policy makers in Ethiopian Health Ministry”.
INDIA
The Government of India funded the National Knowledge Platform, which will help to identify health policy and research priorities in the country. The idea for the Platform emerged from a 2013 Alliance-supported project and subsequent interactions with the Ministry of Health and Family Welfare. In 2018 the Platform was officially launched with a funding commitment of US$ 2.8 million and a secretariat in the National Health Systems Resource Centre.
INDONESIA
The primary health care systems (PRIMASYS) case studies have been used by WHO and its partners to develop cost estimates for essential primary health care services, including a pilot phase in Indonesia.
SOUTH AFRICA
The Alliance-supported review centre in South Africa contributed to the development of WHO guidelines on digital health interventions for sexual, reproductive, maternal, newborn, child and adolescent health (SRMNCAH) and health systems strengthening.
The primary health care systems (PRIMASYS) initiative is highlighted as a model for policy-relevant research in the WHO/UNICEF Operational Framework to implement the Astana Vision for Primary Health Care in the 21st Century.
We are committed.
When engaging health systems, the Alliance recognizes that change can take a long time. Sometimes one step forward can result in two steps back. Long-term engagement with particular countries and institutions is often necessary to continue to significantly strengthen health systems.
Presenting small examples year by year can limit our ability to tell these longer-term stories. This year, we are revisiting two cases - reported in previous annual reports - and provide an update on how they’ve evolved over the years.

Peru: Research to understand how best to integrate care for HIV and TB
THE ISSUE
Tuberculosis (TB) accounts for one in five deaths globally for people infected with human immunodeficiency virus (HIV). Screening, preventing and treating TB in HIV patients is therefore of the utmost importance. Since 2004, the World Health Organization has recommended integrating treatment of TB with HIV care, but it has been difficult to implement in many countries, including Peru.
THE RESEARCH
In 2014, the coordinating team of the Ministry’s Strategy for the Prevention and Control of Sexually Transmitted Infections, HIV/AIDS and Hepatitis B received funding from the Alliance to conduct research into programmatic barriers to integrated care for people co-infected with HIV and TB.
The researchers found that patients with co-infection received neither timely nor comprehensive care. It also found that co-infected patients received TB treatment in a primary health care facility, such as the local clinic, and HIV treatment in a tertiary facility, usually a public hospital far from their homes. These findings pointed to the need for a model of integrated prevention and treatment for co-infected patients at the same medical facilities to improve treatment and follow-up care.
This study informed a pilot scheme supported by the Global Fund to Fight AIDS, Tuberculosis and Malaria that tested just such a model. In 2016, these studies resulted in a policy document to the Ministry of Health recommending a new, integrated strategy for the prevention and treatment of HIV/TB co-infection.
THE RESULT
In 2018, with support from the Ministry of Health, Peru’s President Martin Vizcarra announced at the UN Security Council that US$ 121 million had been allocated for improved care for patients with HIV/TB co-infection. That same year, Peru’s government approved the Ministry of Health’s proposed integrated care strategy.
This case study illustrates the importance of embedded research and locally-driven policy processes. Although the WHO had advocated for integrated care for people co-infected with HIV and TB, the research to understand how to do that in Peru was critical for informing this new national policy.
THE ISSUE
In 2005, Nigeria implemented a national immunization strategy that resulted in an overall increase in vaccination rates. A decade later in Ogun State, though, only 12 of the 20 local government areas (LGAs) had reached full immunization coverage. The other eight LGAs saw little improvement and continued to have large pockets of unimmunized children.
THE RESEARCH
To understand better what was occurring in these LGAs and to try to find ways of improving vaccination coverage rates, the Ogun Primary Health Care Development Board, local academic institutions, and the Royal Tropical Institute in the Netherlands (KIT) proposed an investigation of the issue in two wards in Remo North: Ipara and Ilara. The idea was to take a participatory action research (PAR) approach involving dialogue and action between community members, health workers and local government officials to improve access to and use of immunization services in these wards. The research project was embedded into the National Programme on Immunization in these focal wards and received funding and support from the Alliance, UNICEF, and Gavi, the Vaccine Alliance. These groups also provided technical support to design, undertake and share findings from the project.
The research found that certain vulnerable groups required special attention from health workers. It also found that men needed to be engaged, as they were typically household decision-makers and the research uncovered specific concerns that they had around adverse effects following immunization (AEFI).
THE RESULT
Based on the team’s findings, health workers and community members focused on these particular populations, visiting households and community meetings to talk about vaccination, perceived barriers and ways to minimize AEFI.
The embedded research project helped bring together key stakeholders to understand and address this pressing issue. As the researchers and implementers were working together, it allowed them to adapt quickly and respond to the barriers identified. And the result was impressive: in the study area, immunization coverage for children above nine months, as assessed by a household survey of caregivers, went from 61% to 91%, and caregiver visits to health facilities for routine immunization services rose from 54% to 83%. The community dialogues also led to spillover benefits beyond the project, such as the return of maternal care services in Ilara.
In addition to supporting this project, the Alliance has helped to expand the networks of the policymakers and researchers involved in this project. They presented the findings as part of the policymaker cohort at the Symposium in Liverpool, and policymakers in other states and national-level policymakers in Nigeria garnered interest in the project and its unique approach – as did policymakers from other countries.
Finances and donors
The Alliance gratefully acknowledges the continued core financial support from the Norwegian Agency for Development Cooperation (Norad), the Swedish International Development Cooperation Agency (Sida), and the United Kingdom of Great Britain and Northern Ireland Department for International Development (DFID).
Other donors and supporters include the Bill and Melinda Gates Foundation, Doris Duke Charitable Foundation, Gavi, the Vaccine Alliance, International Development Research Centre, Canada, UNICEF, USAID, and the Wellcome Trust.
Governing bodies
Alliance Board
CHAIR David H. Peters, Professor and Chair, Department of International Health, Bloomberg School of Public Health, Johns Hopkins University, United States of America
Gail Andrews, Chief Operating Officer, National Department for Health, South Africa
Keshav Desiraju, Former Union Health Secretary, Government of India, India
Diana Pinto, Health Lead Specialist, Division of Health and Social Protection, Inter-American Development Bank, United States of America
Dirk H. Mueller, Senior Health Adviser, Health Research Team, Research and Evidence Division, Department for International Development (DFID), United Kingdom
Kelechi Ohiri, Chief Executive Officer, Health Strategy and Delivery Foundation, Nigeria
Ingvar Theo Olsen, Policy Director, Department for Global Health, Education and Research, Norwegian Agency for Development, Norway
Teresa Soop, Senior Research Advisor, Swedish International Development Cooperation Agency (Sida), Sweden
Naoko Yamamoto, Assistant Director-General, Universal Health Coverage and Health Systems, World Health Organization, Switzerland
Scientific and Techncal Advisory Committees
CHAIR Jeanette Vega, Chief Medical Innovation and Technology Officer, Red de Salud UC CHRISTUS, Chile
Trish Greenhalgh, Professor of Primary Care Health Sciences, Nuffield Department of Primary Care Health Sciences, University of Oxford, United Kingdom
Bocar Kouyate, Director, National Malaria Research and Training Centre, Burkina Faso
Simon Lewin, Senior Researcher, Norwegian Knowledge Centre for the Health Services, Norway
George Pariyo, Senior Scientist, Department of International Health, Bloomberg School of Public Health, Johns Hopkins University, United States of America
Sabina Faiz Rashid, Dean and Professor, James P Grant School of Public Health, BRAC University, Bangladesh
Helen Schneider, Professor, School of Public Health, University of the Western Cape, South Africa
Göran Tomson, Professor, Karolinksa Institutet; Senior Advisor, Swedish Institute for Global Health Transformation (SIGHT), Royal Swedish Academy of Sciences, Sweden
Alliance Secretariat
Abdul Ghaffar, Executive Director
Kabir Sheikh, Policy Advisor
Lydia Bendib, Technical Officer
Priscilla Cleland, Administrative Assistant
Veloshnee Govender, Technical Officer
Dena Javadi, Technical Officer
Gloria Kelly, Programme Officer
Jeff Knezovich, Technical Officer, Partnerships and Engagement
Etienne Langlois, Technical Officer
Arielle Mancuso, Technical Officer
Pauline Bempong Administrative Assistant
Ellen Rosskam, Lead, Policy Outreach
Zubin Shroff, Technical Officer
John Warriner, Technical Officer
NOTE: People listed in this section served on the Board or STAC or were employed by the Secretariat at some point during 2018. They do not necessarily reflect the current composition of these bodies.
© World Health Organization 2019
This work is available under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization.
Suggested citation. Annual Report 2018: Alliance for Health Policy and Systems Research. Geneva: World Health Organization; 2019 (WHO/HIS/HSR/19.1). Licence: CC BY-NC-SA 3.0 IGO.
Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. To submit requests for commercial use and queries on rights and licensing, see http://www.who.int/about/licensing.
Third-party materials. If you wish to reuse material from this work that is attributed to a third party, such as tables, figures or images, it is your responsibility to determine whether permission is needed for that reuse and to obtain permission from the copyright holder. The risk of claims resulting from infringement of any third-party-owned component in the work rests solely with the user.
General disclaimers. The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of WHO concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted and dashed lines on maps represent approximate border lines for which there may not yet be full agreement.
The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by WHO in preference to others of a similar nature that are not mentioned. Errors and omissions excepted, the names of proprietary products are distinguished by initial capital letters.
All reasonable precautions have been taken by WHO to verify the information contained in this publication. However, the published material is being distributed without warranty of any kind, either expressed or implied. The responsibility for the interpretation and use of the material lies with the reader. In no event shall WHO be liable for damages arising from its use.
The photographs used in this report were either supplied directly by their subjects or are available in the public domain.
Design and layout by Michelle Samplin-Salgado, Miami Beach, FL, United States.
Printed by the WHO Document Production Services, Geneva, Switzerland.